Toxicology of Coumarin
Coumarin poses significant health risks. Ingestion, inhalation, and eye contact are hazardous, while skin contact is less severe. Acute overexposure can be fatal. Coumarin shows moderate toxicity to liver and kidneys, with a median lethal dose of 275 mg/kg. Hepatotoxicity is more pronounced in rats than mice.
Toxicological data (LD50) for coumarin are:
- 293 mg/kg (rat)
- 196 mg/kg (mouse)
- 202 mg/kg (guinea pig)
Cassia bark, a cinnamon variety, contains highlevels of coumarin. Consuming excessive amounts of cassia bark can be harmful due to its elevated coumarin content.
The U.S. Food and Drug Administration has banned the direct addition of coumarin to food products. Nevertheless, coumarin-containing natural additives, such as sweet woodruff, are permitted in alcoholic beverages under specific regulations.
1. Exposure Routes
Human exposure to coumarin primarily occurs by dermal contact with perfumes and products containing coumarin fragrance. The skin readily absorbs coumarin, making it an important delivery route for therapeutic applications like lymphedema treatment.
Additionally, human exposure can occur by oral ingestion through natural foodstuffs, pharmaceuticals, and tobacco products. Gastrointestinal absorption of coumarin is rapid.
2. Toxicokinetics
Extensive research has described coumarin’s absorption, metabolism, and excretion. Exposure route significantly influences blood levels and toxicity.
Oral bolus doses result in plasma concentrations clearly higher than those observed from dietary intake, despite equivalent milligram-per-kilogram body weight levels.
Dermal exposure bypasses initial liver metabolism (first-pass effect). Coumarin in the blood first passes through the lung, where a significant portion can be exhaled before hepatic metabolism.
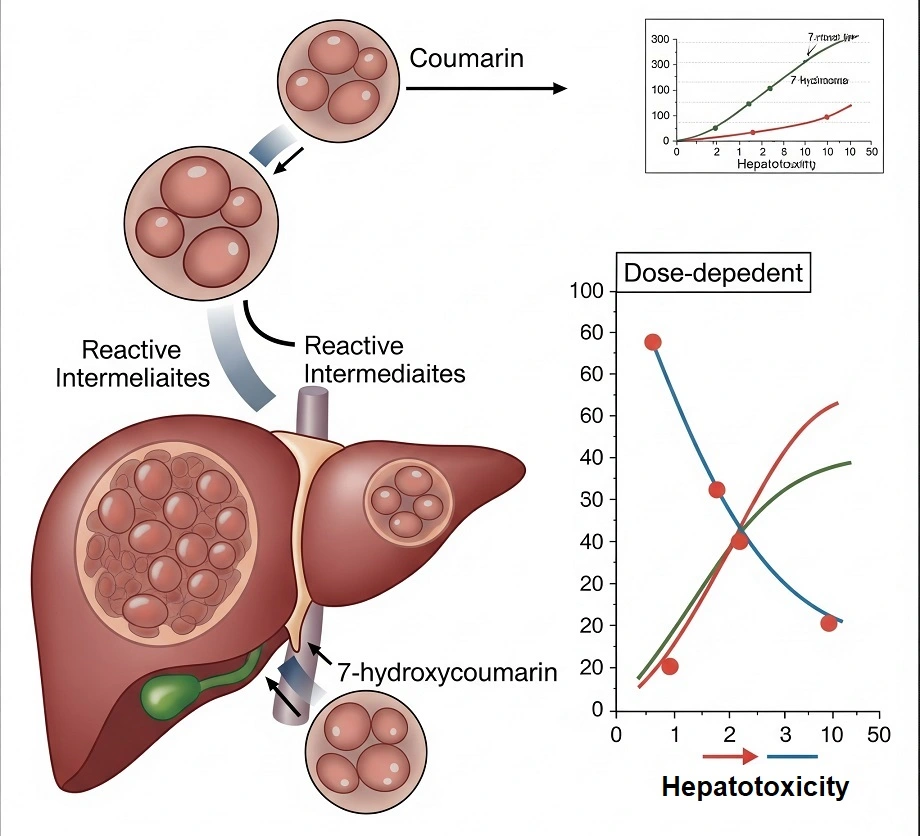
Humans primarily metabolize coumarin to nontoxic 7-hydroxycoumarin. Hepatic formation of o-hydroxyacetic acid is minimal and rapidly detoxified. The absence of abundant Clara cells in human lungs prevents pulmonary epoxide and o-hydroxyacetic acid generation, even at high coumarin doses.
Studies using human hepatic microsomes correlate low 7-hydroxylation capacity with reduced epoxide formation.
3. Acute and Short-Term Toxicity
3.1. Animal Studies
Reported LD50 values for coumarin range from 160 to 780 mg/kg body weight, with variations attributed to animal species, strain, and fasting status. Mild eye and skin irritation has been observed after exposure.
Dietary exposure to coumarin at levels ≥2500 ppm for at least four weeks can lead to decreased food consumption, reduced body weight, and microscopic liver changes. Higher dietary concentrations (1-2%) result in food refusal and mortality.
Reproduction may be adversely affected at high-dose levels that significantly impact food consumption, but no reproductive or developmental effects have been reported at lower doses.
3.2. Human Studies
Human exposure to coumarin occurs through the consumption of cinnamon, green tea, sweet clover honey, and other foods. Cases of bleeding associated with herbal teas containing tonka beans, melilot, and sweet woodruff have been reported.
Pharmaceutical coumarin dosages range from 70 to 7000 mg/day, with 200 mg once or twice daily being the most common regimen.
Hepatotoxicity has been infrequently reported following pharmaceutical coumarin use. Associated hepatic enzyme changes are often reversible upon treatment cessation and sometimes even while continuing treatment.
Reported incidence rates vary from <0.1 to 6%, influenced by the study population and dosage. Although some deaths have been linked to coumarin use, confounding factors such as pre-existing medical conditions complicate causal interpretation.
Studies investigating the CYP2A6 polymorphism in humans have not established a connection with coumarin-associated liver dysfunction.
Coumarin has undergone sensitization testing in various models, including guinea pig dermal application, mouse ear swelling test, and local lymph node assay (LLNA). Pure coumarin consistently yielded negative results, even at concentrations up to 50% in recent LLNA studies.
However, a chlorinated impurity (6-chlorocoumarin) and less-pure coumarin derived from o-cresol have demonstrated sensitizing properties, aligning with reported sensitization cases involving coumarin derivatives.
Human populations, unlike laboratory animals, may have pre-existing exposure to coumarin or cross-reactive substances, complicating human sensitization assessment.
Coumarin’s anticoagulant activity is significantly lower than that of warfarin. Case reports suggest coumarin may potentiate the effects of vitamin K antagonists, although the underlying mechanism remains unclear. Coumarin has not been associated with teratogenicity or adverse reproductive effects in humans.
4. Chronic Toxicity
4.1. Animal Studies
Extensive long-term toxicity and carcinogenicity studies on coumarin have been conducted. The primary adverse effects observed in animals are decreased food consumption leading to reduced body weight and liver toxicity, particularly in rats.
Liver tumors, although non-metastatic and non-lethal, have been reported in rats exposed to high doses (≥150 mg/kg body weight) that significantly reduced body weight gain. Lung tumors have been identified in mice exposed to high bolus doses (≥150 mg/kg body weight) but not in those exposed through diet.
4.2. Human Studies
Occupational exposure to coumarin dust may cause respiratory irritation. Additionally, coumarin may act as a weak dermal sensitizer in susceptible individuals, with the degree of sensitization influenced by the substance’s purity. No other long-term adverse effects in humans have been documented.
The International Agency for Research on Cancer (IARC) has classified coumarin into Group 3, indicating it is not classifiable as a human carcinogen.
In Vitro Toxicity
Coumarin is not mutagenic and does not bind to DNA. It shows no clastogenic properties, indicating a negligible impact on chromosomes.
Reproductive Toxicity
Unlike warfarin, coumarin is not teratogenic.
Genotoxicity
Multiple studies have consistently shown that coumarin is not genotoxic. It has exhibited protective properties against doxorubicin-induced mutations.
Carcinogenicity
There is no conclusive evidence to classify coumarin as a carcinogen. In fact, some research suggests potential antioxidant and antineoplastic effects.
Clinical Management of Overdose
Due to the relatively low toxicity of coumarin, specific overdose management protocols are limited. General measures, such as gastric decontamination in cases of significant oral ingestion, may be considered. Monitoring of international normalized ratio and liver function tests is recommended.
Ecotoxicity
Coumarin exhibits low environmental toxicity. Aquatic toxicity studies have shown LC50 values of 56 mg/L for fish and EC50 values of 55 mg/L for Daphnia magna. Algal respiration is inhibited at laboratory concentrations of 50 mmol/L.
Given its relatively low persistence, coumarin is expected to readily degrade in the environment.
References
- Coumarin; Kirk‐Othmer Encyclopedia of Chemical Technology. – https://onlinelibrary.wiley.com/doi/10.1002/0471238961.0315211302150919.a01.pub2
- Coumarins. – https://www.sciencedirect.com/science/article/abs/pii/B9780123864543007983
- https://www.sciencedirect.com/science/article/abs/pii/B0123694000002696
- https://onlinelibrary.wiley.com/doi/10.1002/mnfr.200900281
- https://www.sciencedirect.com/science/article/abs/pii/B9780124095472126204
- https://pubchem.ncbi.nlm.nih.gov/compound/Coumarin
